October 20, 2023 | AI and NLP, Quality Improvement, Year Round Prospective HEDIS®
Take Prospective HEDIS® to the Next Level with An Effective Leads Program
For those Health Plans that are already implementing a prospective, measurement-year program to close HEDIS® gaps across your populations – know that you are taking one of the most important first steps towards Digital Quality, by realigning your workforce to a full-year HEDIS® quality process and taking the sting out of the loss of the hybrid methodology.
If you’re using natural language processing (NLP) to help you identify compliant members and exclusions, you can effectively multiply the strength of your team by a factor of seven. As your prospective program gains strength, you will rely less and less on the sample, achieve higher rates, and better manage your populations with less provider and member abrasion.
More advanced teams are ready to take the next step, which is the subject of this blog.

Rebecca Jacobson, MD, MS, FACMI
Co-Founder, CEO, and President
How do you create value from gaps that are classified as “leads”, maximizing compliance during the measurement year, when both health plan and provider can be most effective?
What’s a Lead?
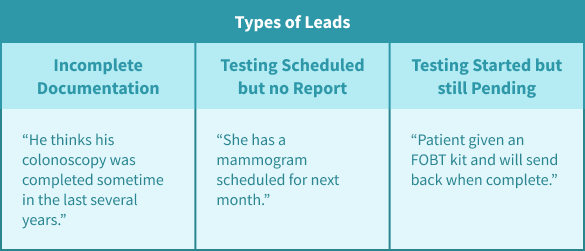
Let’s first start by defining a lead. In Astrata’s Chart Review system, a lead refers to a gap that we classify as having some but not all the evidence needed to close the gap. In some cases, the gap is actually a Hit, but our NLP system doesn’t have sufficient confidence to label it as a Hit. Your abstractors can close these gaps. In other cases, the gap is really a quality improvement opportunity, and while you can’t close it just yet, you might be able to with a bit more work.
In this blog, we will focus on the latter set of gaps – to learn how you can further advance your quality improvement programs by separately working this leads queue.
Lead Examples
- Incomplete Documentation: “He thinks his colonoscopy was sometime in the last several years.”
- Testing Scheduled but No Report: “She has a mammogram scheduled for next month.”
- Testing Started but Still Pending: “Patient given an FOBT kit and will send back when complete.”
Why are Leads Important?
Leads are important for several distinct reasons. Let’s dive a bit deeper into the types of leads described above.
First, they represent a set of members who very well may be compliant, but for whom you are not able to “close the gap”. And in that sense, they’re low-hanging fruit as you find yourself looking for additional gap closures to help you achieve the target you may be aiming for given your current rate and cut-point projections. The first lead in the graphic describes a colonoscopy with no date — and that can’t be used as evidence based on the HEDIS spec. But it does open the door to a conversation directly with a provider, or through your practice-based care managers to correct this documentation miss.
Second, leads can also tell you when the appropriate intervention has been ordered by the provider but you don’t yet have the results. For example, in the second lead above, it’s appropriate to wait a month and then follow up if the member still has no mammogram claim or result. But in the third lead, the member may need a reminder to return the FOBT or FIT DNA kit.
In all three cases, your probability of closing one of these gaps is much higher than any random gap. By working the leads queue, your team can further optimize your efficiency, focusing on the gaps that have the most potential to improve member management and produce higher rates. As you start to distinguish truly open gaps from leads, you can also provide this data back to your providers to help them respond appropriately.
Best Practices for Optimizing Your Leads Program
1. Work a Distinct Leads Queue with the Right Personnel
By using natural language processing products (like ours), you can effectively identify leads, separating them from hits and exclusions that your abstractors need to close, as well as real gaps that will flow back to your providers using your existing processes. Lead queues can be independently worked with the correct staff, which may be quality improvement or care management teams in larger organizations.
2. Address Documentation Problems at Multiple Levels
Cases that represent missed documentation can be worked in multiple ways – by providing specific gap insights directly, and by using your provider education teams to address challenges.
3. Identify QI Opportunities that Have Outsized Impact
Knowing where to spend your time and energy is a critical part of developing a successful leads program. Your HEDIS and Stars analytics can help you identify the most important measures to be working, based on your current rate, and predicted cutpoints.
Leads are Part of the QI Continuum
Always keep in mind that leads are part of the continuum of QI opportunities, which also include surveillance measures such as Osteoporosis Management in Women (OMW), where the goal is to identify non-compliant members prior to receiving a claim for the fracture and identifying them as non-compliant. By running your measures in “surveillance mode” you can identify opportunities for rapid response for noncompliant members, preventing further complications (such as secondary fractures), and reducing avoidable costs.
The Next Big Thing – Get Your Gaps Directly to the Point of Care
We’re excited to be working with our partners at HOLON to deliver Astrata’s “smart gaps” directly into electronic health records, through the HOLON ribbon. We’ll be sharing more about this exciting collaboration in the near future.
By pushing your quality gaps into the clinical workflow, instead of through a separate portal, you’ll see the potential for transformational change in payer-provider collaboration.
